COARCTATION OF AORTA DIAGNOSED BY RENAL DOPPLER
IN A HYPERTENSIVE CHILD
Coarctation of the aorta
is an abnormal narrowing of the aorta
that occurs as a result of persistent muscular tissue in the region of the
ligamentum arteriosus. Coarctation most commonly seen opposite the ductus arteriosus, caudal to origin
of the left subclavian artery and is called juxta-ductal coarctation.
Coarctation is a cause of secondary hypertension, resulting in differential
pressures in the upper and lower extremities.
CASE DETAILS
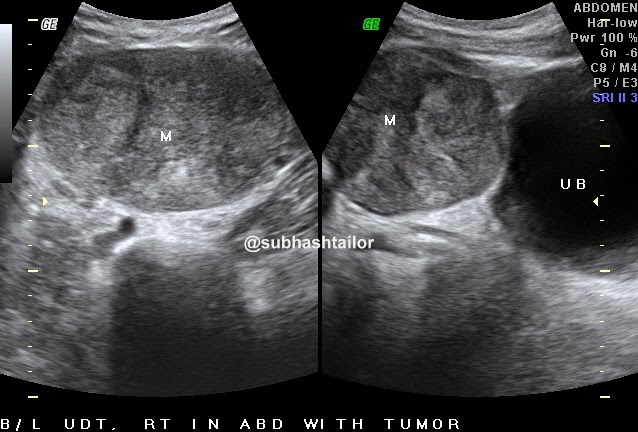
A13 yr young boy with
hypertension [ BP upper limb 150/98] , subjected to abdominal ultrasound with
special study for renal Doppler . Abdominal organs were normal at USG. On renal
Doppler examination both sided main renal arteries were poorly seen & could
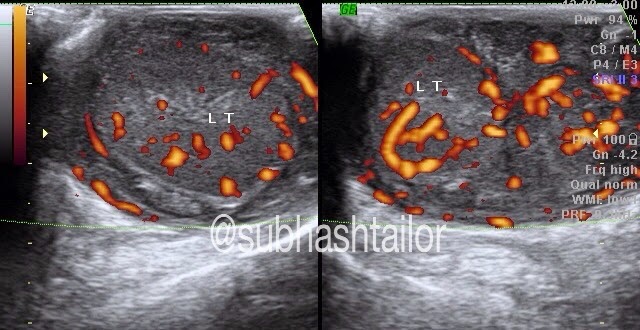
not be clearly scanned. However in this case study a low velocity low resistance tardus -parvus waveform is seen in both sided
intrarenal renal arteries [fig 1 & 2 ]. The parvus tardus waveform of the renal
artery is characterized by a slow rise of peak velocity distal to the stenosis,
prolonged acceleration time and reduction of ipsilateral resistive index. This suggested
that a stenosis proximal to the point being studied may be present. The
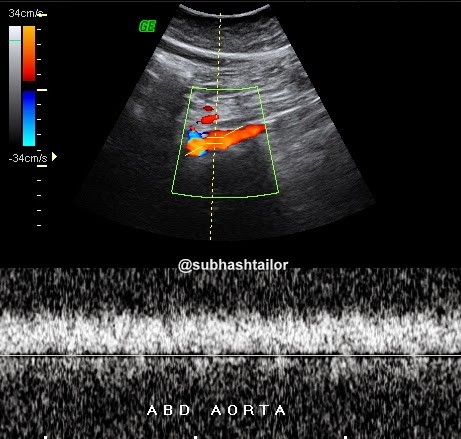
supra-renal aorta showed a monophasic and dampened flow due to low flow
velocities [ fig 3 ], further suggesting that a more proximal narrowing is likely , &
that could be coarctation of aorta . So , a possible diagnosis of coarctation
of aorta was proposed . Further
examination by CT scan confirmed the
presence of juxta-ductal coarctation [ fig 4 & 5 ].
Fig 1- Right intrarenal doppler shows tardus-parvus flow pattern . Note the decreased arterial peak systolic velocity & prolonged systolic peak acceleration time , which indicates proximal stenosis
Fig 2- Left intrarenal arterial doppler with similar tradus-parvus flow pattern
Fig 3 - Abdominal aortic doppler scan shows dampened monophasic blood flow spectrum due to low velocities , suggesting more proximal stenosis
Fig 4- Sagittal CECT chest shows aortic stenosis [ c ] in juxta ductal isthmus of aorta [ AO ] caudal to left subclavian artery
Fig 5 - Coronal CECT chest shows juxta ductal aortic stenosis
Take
home point from this case: Look for a more proximal stenosis when
abnormal bilateral renal artery waveforms [ tardus-parvus ] and abnormal aortic
waveform [ dampened ] are noted.
PS – The case study in intended for medical professionals
& imaging specialists for academic purpose