Epiploic appendages are peritoneal pouches that arise from the serosal surface
of the colon. These are composed of adipose tissue and attached to colon by
vascular stalk , multiple in count [ approx 100 ] ,& have
a length range of about 0.5–5 cm. Those
located near the sigmoid colon are the largest in size . Epiploic appendages
are usually not found near the rectum. The appendages are arranged in two rows:
one row medial to the tenia libera, and the other lateral to the tenia
omentalis of the colon .
Epiploic appendagitis is an uncommon self
limiting inflammatory or ischaemic
condition affecting the colonic epiploic
appendage. Appendagitis may be primary[ spontaneous ] or secondary to
adjacent pathology , with more affection or predilection for sigmoid colon ,
presumably due to larger appendices. The condition most commonly manifests in
the 4th to 5th decades of life, predominantly in men & obese individuals . Torsion
of epiploic appendage pedicle , with resultant vascular occlusion or venous
occlusion that leads to ischemia[ ischemic necrosis], has been implicated as
the cause of acute epiploic appendagitis. Acute epiploic appendagitis is also seen to be
associated with hernia, and unaccustomed
exercise. Mostly it is a self limiting disease
, and very uncommonly it may
result in adhesion, bowel obstruction, intussusception, intraperitoneal loose
body, peritonitis, and/or focal abscess formation.
Clinically patients
present with acute abdominal pain and guarding in local area at the site of
involvement [ that is usually lower quadrant , more common in left iliac fossa]
. On the basis of clinical manifestations alone, acute epiploic appendagitis is
mis-diagnosed in most of the cases , and or often its being mistaken for acute
diverticulitis. Unlike acute epiploic
appendagitis, acute diverticulitis is more likely to cause evenly distributed
lower abdominal pain and associated with
nausea, fever, and leukocytosis. On the
contrary most patients with acute epiploic appendagitis do not manifest any change in their bowel habits, and only a
few cases report constipation or diarrhea.
Differential diagnosis ;
1] acute omental infarction
2] diverticulitis
3]sclerosing mesenteritis or mesenteric
panniculitis
4] primary tumor or metastasis that involves
peritoneum and mesocolon.
Ultrasound
Findings
The site of maximum tenderness[mostly left iliac fossa] is the
region of interest for ultrasound evaluation . There is evidence of a round to
oval echogenic noncompressible mass noted , with no internal vascularity on
doppler, and surrounded by a subtle hypoechoic line . The lesion is typically 2 - 5 cm in maximal diameter
adjacent and anterior to colon , and just deep to abdominal wall . The mass
exert slight compressive effect on colonic loop
, and usually not associated with
colonic mural thickening , or local or
free peritoneal fluid .
In my
series of 7 patients [ 6 M &
2F, age range 35 to 48 yrs] , six cases presented with pain left iliac fossa ,
& one case with pain in right iliac fossa.
All cases were showed classical ultrasound findings of epiploic
appendagitis with no bowel thickening or ascites . In all cases no leucocytosis
was observed in lab. tests. In one case with pain right iliac fossa , the d/d
was with acute appendicitis , but appendix and ileo-cecal region was seen
separately & normally on ultrasound
.
Fig 1- Shows a normal descending colonic epiploic appendage : An oval elongated echogenic structure [ arrow] attached to DC loop, nicely depicted due to presence of ascites[FL]
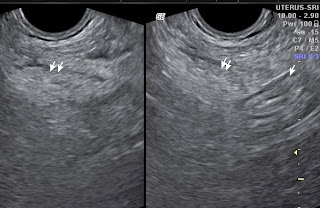
Fig 2 - Epiploic appendagitis, case A : LIF scan shows a well defined oval echogenic mass [bet cursors] surrounded by hypoechoic halo , just deep to abd wall
Fig 3 - LIF scan of same case A , mass with no internal vascularity on power doppler
Fig 4 - CT scan sagittal reconstruction image of case A, shows a well defined oval hypodense fat density lesion along descending colonic loop[arrow within circle]
Fig 5 - Epiploic appendagitis, Case B, LIF scan shows a well defined oval echogenic mass[ twin arrow] between sigmoid loop[single arrow] and abd wall
Fig 6 - Epiploic appendagitis, case C, LIF scan shows an oval echogenic mass with hypoechoic rim[arrows] adjacent to normally appearing sigmoid cooln
CT
findings-
A fat-density ovoid lesion adjacent to colon, size varying 1.5 - 3.5cm in
diameter , with thin high-density rim , surrounding inflammatory fat
stranding, and thickening of the adjacent peritoneum. A central hyperdense dot like
area also appreciated representing the thrombosed vascular pedicle. As a chronic
sequele an infarcted appendix epiploica may calcify, and may detach to form an
intraperitoneal loose body.
Treatment
and prognosis
Epiploic appendagitis is a
self limiting disease, and thus a correct diagnosis is important with imaging
modalities to prevents unnecessary surgery.
Ref.





.JPG)




.jpg)
.jpg)
.jpg)
.jpg)
















































