Image Presentation
ACUTE SEGMENTAL TESTICULAR INFARCT -
mimic like a tumor on grayscale ultrasound , and color Doppler
ultrasound can clearly differentiate it
from tumor .
Abstract
Segmental
testicular infract is very uncommon pathology , & involves variable etiology
, but commonly idiopathic . On grayscale ultrasound it appears
as a focal inhomogenic mass which is difficult to be differentiated from testicular tumor . However high
resolution color Doppler ultrasound confidently
diagnose it as an area of infarction & allows testis sparing surgery .
Introduction
Color Doppler
ultrasound ( CDUS ) is very useful modality in evaluation of acute scrotum ,
and to differentiate between epididymoorchitis & torsion when
symptoms may overlap ( 2 ) . The common conditions causing a painful
scrotum includes torsion & epididymoorchitis
, and rarely tumor . Testicular tumor
normally presents as a slow growing mass , rarely painful , and incidently
discorved by the patient( 3 ) . On
grayscale ultrasound tumor appears as an inhomogenic focal mass and CDUS
demonstrates internal vascularity with malignant vascular pattern ( 4 ) . I
present a case with painful testicular focal inhomogenic mass on grayscale
ultrasound where CDUS allowed the diagnosis of segmental testicular infarction , rather than a testicular tumor , to be labelled .
Case report
A 46 years
old man presented with a history of increasing right testicular pain for few
days . The case was already on
antibiotics for presumed epididymoorchitis , however with no significant relief
. On physical examination there was tenderness at the upper pole of right
testis and epididymis , and a clinical diagnosis of epididymoorchitis was made. In view of no relief in symptoms , the
scrotal sonography was requested . Scrotal sonography was performed on GE –
Logiq 400 pro ultrasound system , using
8 to 11 MHZ. linear probe with small parts setting . The grayscale ultrasound
examination revealed a focal enlarged inhomogenic area of iso to hypoechoic echogenisity at upper pole of right testis ( figure 1 ) .
The CDUS failed to show any color flow signals within the mass but color flow
signals were noted normal in rest of the testicular parenchyma ( figure 2 ) . No any calcific focus or cystic change noted
within lesion . No any other ultrasound evidence of epididymoorchitis was present
. The possibility of an acute segmental testicular infract was made rather then
a tumor because of absent color doppler signals in the focal abnormal area .
The patient had normal complete blood count , and was advised surgical exporation by the referring doctor to exclude spermatic
cord torsion as a cause for the abnormality . But the patient had refused for surgery , and was allowed to continue symptomatic medical treatment
for some days .
After few
weeks the referring doctor was contacted for follow up details of this case ,
and he ( referring doctor ) confirmed
that the patient improved gradually and became symptom free with some residual
testicular atrophy . The patient was advised
a review ultrasound but he did not turn
up .
Discussion
Total
testicular infarction is usually seen after torsion of spermatic cord , severe
epididymoorchitis or trauma ( 2 ) . Segmental testicular infarction is a rare entity and usually diagnosed by postorchidectomy
histopathology ( 5, 6 ) . The
predisposing factors to segmental infarction includes polycythemia ( 7 ) , intimal
fibroplasia of spermatic artery ( 8 ) , sickle cell disease ( 9 ) ,
hypersensitivity angitits ( 10 ) and trauma , although most of the cases are
idiopathic in origin ( 7 ) , as in this case . S. Sriprasad et. al. reported a case in BJR in 2001 with the same grayscale and CDUS findings , which was proved to be a segmental
testicular infarct histopathologically .
Scrotal sonography is valuable tool in differential diagnosis of acute scrotum , & clearly differentiate
testicular torsion & infarct with
high accuracy . In epididymoorchitis the testis and epididymis shows hyperemia
, whereas absent or poor vascularity seen in torsion and infarct . The B- mode
findings in acute testicular ischemia are enlarged and hypoechoic testis . CDUS
helps to diagnose testicular torsion
where absent or poor blood flow noted in symptomatic testis , and normal blood flow in contralateral testis . The testicular tumors are usually seen
as focal inhomogenic or variable echotexture
masses with disordered / malignant
internal vascularity on Doppler ( 13 ) .
On color Doppler , focal lesions larger than 16 mm , usually show raised and
disordered blood flow ( 4 ) . Segmental testicular infarct also appears as focal
mass of variable echogenicity with absent blood flow on Doppler ( 1 ) . However cases with focal area of increased
echogenicity and poor or absent blood
flow on CDUS were also reported and documented in
segmental infarct ( 16 ) . This case showed focal inhomogenic or variable echotexture mass
at upper pole right testis with absent blood flow signals on CDUS , closely
resembles the case reported by S. Sriprasad
et. al. . There was focal
enlargement of upper pole of testis , which may indicate acute nature of the disease , because in chronic process the
affected testis may appear small or shrunken ( 16 ) . So with recent advances in probe technology
and color Doppler sensitivity , it is
possible to document Intratesticular blood flow as well as vasculature pattern
in a better way , which is important particularly
in differentiating a malignant mass from segmental infarction , as both appears
identical on B – mode ultrasound , and thereby helpful in suggesting a treatment planning ( testis sparing & conservative
management ) .

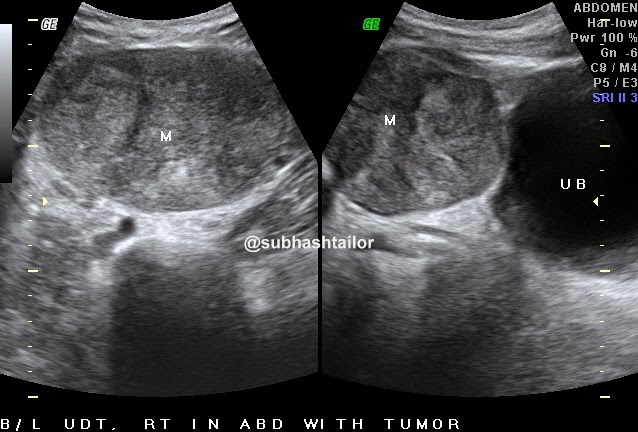
( Figure 1
) - Sagittal US image shows
inhomogenic iso to hypoechoic mass like lesion
( two small arrows )
involving upper pole of right testis
( Figure 2
) -
Color Doppler Us image of same testis shows absent color flow signals in
the abnormal area s/o infarct , and
normal blood flow signals in rest of the testis .
PS ; The case study is based on imaging features & review literature , and intended for medical professionals & imaging specialists for academic purpose .
Referrences
1. S .sriprasad et al. Acute segmental testicular infarct : differentiation from tumour using high
frequency colour Doppler ultrasound. BJR [74]2001,965-967
2. Sidhu PS. Clinical
and imaging features of testicular
torsion: role of ultrasound. Clin Radiol 1999;54:343–52.[Medline]
3. Morse MJ, Whitmore
WF. Neoplasms of the testis. In: Walsh PC, Stamey TA, editors. Campbell's
Urology (5th edn). Philadelphia, PA: WB Saunders Co., 1986:1535–82.
4. Horstman WG, Melson
GL, Middleton WD, Andriole GL. Testicular
tumours: findings with color Doppler US. Radiology 1992;185:733–7.[Abstract/Free Full Text]
5. Han DP, Dmochowski
RR, Blasser MH, Auman JR. Segmental infarction of the testicle: atypical
presentation of a testicular mass. J
Urol 1994;151:159–60.[Medline]
6. Costa M, Calleja R,
Ball RY, Burgess N. Segmental testicular infarction.
BJU Int 1999;83:525.[Medline]
7. Jordan GH. Segmental hemorrhagic infarct of testicle. Urology 1987;29:60–3.[Medline]
8. Brehmer-Andersson E,
Andersson L, Johansson J. Hemorrhagic infarctions
of testis due to intimal fibroplasia of spermatic artery. Urology
1985;25:379–82.[Medline]
9. Holmes NM, Kane CJ. Testicular infarction
associated with sickle cell disease. J Urol 1998;160:130.[Medline]
10. Baer HM, Gerber WL,
Kendall AR, Locke JL, Putong PB. Segmental
infarct of the testis due to
hypersensitivity angiitis. J Urol 1989;142:125–7.[Medline]
11. Martin B, Conte J.
Ultrasonography of the acute scrotum. J Clin Ultrasound 1987;15:37–44.[Medline]
12. Middleton WD, Melson
GL. Testicular ischemia: color
Doppler sonographic findings in five patients. AJR 1989;152:1237–9.[Abstract/Free Full Text]
13. Grantham JG,
Charboneau JW, James EM, et al. Testicular
neoplasms: 29 tumors studied by high-resolution US. Radiology 1985;157:775–80.[Abstract/Free Full Text]
14. Gofrit ON, Rund D,
Shapiro A, Pappo O, Landau EH, Pode D. Segmental
testicular infarction due to sickle cell disease. J Ultrasound Med
1998;160:835–6.
15. Flanagan JJ, Fowler
RC. Testicular infarction mimicking tumour on scrotal
ultrasound: a potential pitfall. Clin Radiol 1995;50:49–50.[Medline]
16. Kramolowsky EV,
Beauchamp RA, Milby WP. Color Doppler ultrasound for the diagnosis of segmental testicular
infarction. J Urol 1993;150:972–3.[Medline]
17. Bushby L, Sriprasad
SI, Sidhu PS. Focal testicular
abnormalities: evaluation of lesion vascularity using high frequency colour
Doppler ultrasound. Eur J Ultrasound 2001;13:S30.